Temporal bias occurs when we assume a wrong sequence of events which misleads our reasoning about causality. It mostly affects study designs where participants are not followed over time.
The most common study designs that are subject to temporal bias are:
- Cross-sectional studies: Because information is collected at a single moment in time
- Case-control studies: Because information is collected retrospectively
When researching a causal relationship between a risk factor and a disease, it is important to determine which occurs first. If you’re only interested in the correlation between them, then you don’t have to worry about temporal bias — Temporal bias can only be a threat when inferring CAUSAL relationships.
Example of temporal bias
Does your level of education affect your health? Or is it the other way around?
Let’s find out!
A lot of research has been done to study the relationship between education and health.
In a nutshell, it is well known that a lower education level is CORRELATED with poor health.
Correlation, however, is like equality:
x = y also means that y = x
It doesn’t tell us anything about the causal relationship between both sides of the equation.
So a correlation between education and health can be the result of:
- Education influencing health
- Health influencing education
- Non-causal relationship between education and health (another example of non-causal relationship would be that between foot size and IQ in children)
We will represent the correlation between education and health as a double-headed arrow:
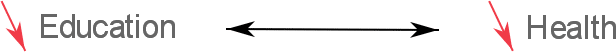
However, because chronic diseases and bad health in general are problems that affect adults more than school children, there is reason to believe that education/schooling comes BEFORE health problems.
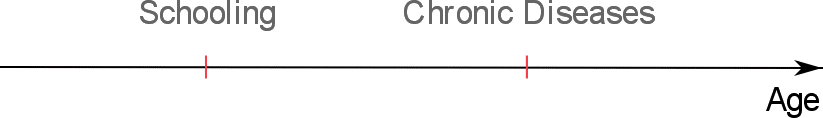
If this is true, then it’s education that influences health and not so much the other way around:
Many studies hypothesized as to why this might be the case:
- Workers with higher levels of education are more likely than others to have employer-provided health insurance [Source]
- Higher levels of educations gives access to healthier neighborhoods [Source]
- Education can help develop cognitive skills that affect health [Source]
But, this is not the end of our story. And here’s where temporal bias comes into play:
It turns out that not all the association between education and health can be explained by our previous model (which states that education influences health).
And we can prove this with evidence from several cohort studies that followed children over time and examined cases where disease actually came BEFORE schooling.
These studies found that:
- Chronic illnesses in young children reduced school readiness [Source]
- Chronic diseases also affect performance in primary school [Source]
- Emergency hospital admissions during childhood increase the risk of lower education attainment [Source]
- Also, Children with attention-deficit/hyperactivity disorder are more likely to have poor long-term school outcomes [Source]
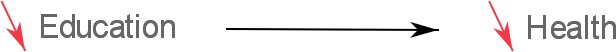
Therefore, some of the strength of the correlation between education and health comes from the reverse relationship of health influencing education:
This phenomenon where the causality arrow is pointing in the opposite direction of common belief is labeled reverse causation.
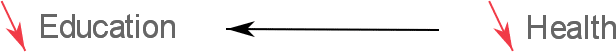
In conclusion, the relationship between education and health has no simple explanation.
The arrow of causality points in both directions as both of these variables influence each other:

How to avoid temporal bias
Here are 2 main solutions for temporal bias:
1. Use a prospective study design
The most effective way to avoid temporal bias is to run a prospective study that follows exposed and non-exposed participants in time and reports which group is more likely to develop the disease.
Examples of prospective studies are: randomized controlled trials and prospective cohorts.
Using such designs, you’ll be certain that the exposure occurs before the disease.
Limitations: If you’re dealing with a rare disease, you’ll have to follow people for a long period of time which can be both expensive and time consuming.
2. Ask for information about the temporal sequence in your questionnaire
In cross-sectional surveys it is possible to ask for information about the temporal sequence between risk factor and disease.
For instance you may ask when the participant first contacted the risk factor.
Limitations: Obviously this method is subject to the participant’s ability to remember events (recall bias).
Another problem is that, in certain cases, participants cannot possibly know the date of exposure to the risk factor (for example most people are not aware of the date when they first contracted an infection with Helicobacter pylori as they never had any signs or symptoms from such an infection).